
*NOTICE*
You will be required (annually) to sign an agreement to abide by the policies and procedures found within this employee manual. The acknowledgement will be at the end of the information at the bottom of the page!
Welcome to True North Supports!
In beginning with TNS it is important that you fully understand and are comfortable with your job duties. Your job will consist of working with, or in behalf of the individuals who have a form of disability specific to them. You will need to study and understand each client’s service needs, support strategies, and behavior plans that you work with. Although two individuals may share the same diagnosis of disability, they are different and unique in many ways. These documents will help you better understand how to best help the individuals you serve. They will provide the specific details to their service needs. If there are any questions regarding service needs, or how to particularly help a specific client (that is not already listed in one of the below documents), contact your direct supervisor.
We desire to lead the industry in quality of care. We seek employees who lead in compassion and consistency. These two core values are an integral part of our service plans and structure. What we do can be a lot of fun if employees plan and prepare properly. Please review this handbook as a tool for you to study and refer to throughout your employment with TNS. This will help you approach this job with confidence and consistency.
True North Mission: “To improve the quality of life of the individuals we serve by choosing to be different; by allowing our individuals to make mistakes in order to then learn from them. We all want compassion and understanding in our shortcomings. It is only right that True North’s mission is to provide that same platform for the individuals within our scope of care. It is our greatest effort to afford our individuals the ability to re-align and effectively progress.”
True North Motto: “Seek learning and growth while giving your best effort.”
____________________________________________
Pay Periods & Pay Schedule
W2
1st Pay Period: 1st – 15th | Paid on the 25th of the month.
2nd Pay Period: 16th – 30th or 31st | Paid on the 10th of the following month.
CONTRACT (HHS)
Pay Period: 1st – 31st | Paid on the 15th of the following month.
____________________________________________
Duties and Responsibilities
Job Objective: To support intellectually & developmentally disabled individuals in their development of basic living and social skills with the primary goal of independence and integration into the community to the best of their ability.
REPRESENTATIVE DUTIES:
- Develop service recipient’s basic living skills (e.g., social, domestic, and hygiene) through instruction and encouragement.
- Assist and document the development and implementation of long and short-term goals for service recipient, as developed by the Personal Support Team under the supervision or direction of the Program Coordinator.
- Develop and maintain a positive and effective relationship with service recipients, families, staff, administration, case management, and other service providers and assist in coordinating with any and all their needs concerning service recipients.
- Perform or assist service recipient with personal hygiene as needed (e.g., bathing, brushing teeth, shaving, nail clipping, dressing, bodily functions, and service recipient appearance). Personal care services that are assigned by a health professional may include observation, reporting and documentation of changes in the status of the person or in body functions. This may include reading and recording the person’s temperature, pulse and respirations, and other needed personal care services.
- Perform or assist service recipient in basic domestic duties as needed (e.g., cooking, cleaning, laundry, shopping).
- Coordinate and maintain service recipient’s schedule (e.g., doctor appointments, professional team appointments and job).
- Coordinate service recipient’s participation in leisure and recreational activities.
- Maintain records and complete paperwork as required by DSPD (e.g., time-sheets, mileage, petty cash, medication logs, service recipient progress, Incident Reports and goal data).
- Adhere to service recipient’s behavior and health management plans (e.g., administration of medication, use of behavior modification techniques, dietary restrictions).
- Maintain a safe environment for the service recipient; prevent harm to service recipient, self, and others.
- Report any safety concerns to management in a timely manner.
- Transport service recipient to and from work, scheduled appointments, and recreational activities in a safe and timely manner.
- Serve as a good role model to service recipient.
- Maintain current certification as required by TNS and DSPD.
- Keep up to date with current employee policies and procedures of DSPD, DHS & TNS
- Strictly adhere to TNS money management policies in support of TNS individuals. This included never giving money or ‘gifts’ to TNS individuals, never giving loans of any kind, and never accepting money, gifts or ‘loans’ from the individuals TNS supports.
____________________________________________
Paperwork Policies & Procedures
Paperwork date ranges and due dates:
Time sheets & Shift Data Notes : All shift information and data entry through T-Sheets App is due:
1st Pay-period (1st – 15th): on the 16th before noon.
2nd Pay-period (16th – 31st): on the 1st before noon.
Example: July time sheet and Shift Note’s would be due before 12:00 pm on August 1st.
Support Strategies (SS) & Monthly Summaries
1st – 30th: due on the 5th before noon.
Example: July SS & summaries would be due before 5:00 pm on August 5th.
If forms are late, paychecks may be delayed by one week.
All forms are pdf fillable so paperwork can be completed on a computer, or using your smart phone with the adobe fill and sign app (see training/tutorial) or by hand and scanned (using the adobe scan app) and emailed [email protected].
All paperwork needs to be completely and correctly filled out – you need to contact us during the month if you have questions regarding hours with clients, overtime, or anything else. The end of the month is not the time to notify us of any discrepancies.
____________________________________________
How To View Pay Checks
When you are first hired you will be sent an email with a link that will require you to create a workforce login username and password. Once your login is created you will have access to pay checks and other employment info as needed.
THIS IS A LINK TO WORKFORCE LOGIN PAGE
You will not have access until you have received the email from quickbooks allowing you access to create an account. You can bookmark the above URL to your browser so you have continual access. There is also a link to “View My Paycheck” under “Employee Portal” on the TNS website. This link takes you to workforce login page.
____________________________________________
Lost Check Policy
All employees are required to fill out a direct deposit form with TNS. If there are issues with setting up a direct deposit account with TNS, with prior approval from TNS admin team, you may receive a paper check. If you lose your paper check there is a $20 dollar check cancellation fee. It will be deducted from that current check/pay period. Example: If you lose a $200 check and ask for a rewrite, your new issued check will be $180.
____________________________________________
Money Management Policy
TNS employees will never loan or accept loans of any kind from the individuals they directly or indirectly support. TNS employees must never buy things for TNS individuals (gifts, food, clothing, shoes, electronic devices, etc.) without written permission from TNS executive staff. If TNS is to loan any money to an individual, TNS must follow specific state given requirements and there are no exceptions. Staff will never use their own personal funds for approved client loans. TNS administration will govern all financial interactions between TNS and the individuals the program supports. If TNS were to engage in a loan with any individual, written understanding must be confirmed from Individual’s team members and a plan must be set in place for repayment of the loan. If any loan exceeds $2,000 it is reviewed, in detail, by the Department of Services for People with Disabilities.
It is inappropriate to give individuals money no matter how insignificant it may seem. It is also inappropriate to receive any money/gifts (food, cash, etc.) from TNS individuals and their families.
All employees are required to confirm strict adherence to our money management policy.
____________________________________________
Nondisclosure and Non-competition
- After execution or termination of your employment agreement, employee agrees to respect the confidentiality of TNS’ patents, trademarks and trade secrets and to not disclose them to anyone. This includes but is not limited to salary/hourly pay.
- Employee agrees to not make use of research done in the course of work done for TNS while employed by a competitor of TNS.
- Employee agrees to not set up in business as a direct competitor of TNS within a radius of 100 miles of TNS for a period of 1 year following the expiration or termination of this agreement.
- In the instance that a staff member were to begin their own service provider, staff agrees to not make an attempt to obtain clients directly from TNS. This means staff will not make arrangements or plans with families or clients and that staff agrees to disassociate themselves from all families and clients and to not acquire any client who was with TNS within 2 year of termination of employment and this agreement.
- Employee agrees to pay liquidated damages of $100,000 if any violation of these paragraphs are proved or admitted.
____________________________________________
True North Supports Incident Reporting
If an incident occurs, Staff is required (as soon as safely possible) to notify their direct supervisor, who will pass the information on to the TNS Admin Team. If you cannot reach your direct supervisor contact the TNS admin team at (385) 434-3408. Staff will then complete a DHS/DSPD Form I-8 Behavior | Incident Report and make sure that it gets turned into their direct supervisor before the end of their workday. When there is a reason to believe an incident has occurred such as, abuse, neglect, exploitation, or maltreatment of an adult, staff & the contractor shall immediately notify Utah Adult Protective Services (APS) intake or Child Protective Services (CPS) intake or the nearest law enforcement agency, and shall immediately notify the Division of Child and Family Services (DCFS) intake or the nearest law enforcement agency in a case involving a child.
The following situations are incidents that require the filing of a report:
- When reason to believe an incident of abuse, neglect, exploitation, or maltreatment has occurred per the DHS/DSPD Code of Conduct.
- A Person’s drug or alcohol abuse, medication overdoses, or medication errors requiring medical intervention.
- Instances in which the whereabouts of a Person is unknown for at least two hours or longer.
- Evidence of seizure in a Person with no existing seizure diagnosis.
- Instances of significant property destruction (totaling $500, or more)
- Instances of physical injury to Person’s requiring a medical intervention
- Instances of law enforcement involvement or charges filed surrounding a Person
- Any use of manual restraint mechanical restraints, or use of a time-out room, as defined in Utah Administrative Code, whether outlined in Person’s PSP or not.
- Any use of level II emergency interventions as defined in Utah Administrative Code.
- Any other instances the Contractor determines should be reported.
____________________________________________
Notification Process for Lost Client
In the event of a lost client, there are certain steps that must be followed.
If a client is missing for more than 2 hours, no longer than 24 hours (use your judgment on what you know about the Client):
1.) Notify TNS admin, (385) 434-3408
2.) Fill out a Behavior | Incident report
3.) Prepare to notify the police (locate the client’s reference sheet with their date of birth, physical description, family contact, and a photo if possible). IF it becomes necessary to contact the police, they will need this information.
4.) Stay by your phone and wait for further instructions.
*Keep the TNS admin informed of any communication you receive from the client*
Executive Contacts:
Jake Probert – Executive Director
TNS Admin Email: [email protected]
TNS Admin Phone: (385) 434-3408
When to Call 911/Proper Authorities (APS, DR./Hospital)
When a medical emergency occurs, it’s not always easy to think clearly. But a crisis means that you need to act quickly. Learning about your choices ahead of time will help you when an emergency does happen.
When you need immediate medical help, you have three choices. You can call the 911 emergency number. You can go to a hospital emergency room. Or, you can call your doctor for advice. Here’s a look at which choice is best.
911:
The 911 emergency number-or your community’s local emergency number-is for true emergencies. An emergency threatens a person’s life, limbs, or sense organs. Examples are heart attacks, strokes, breathing problems, head and neck injuries, severe bleeding, and eye injuries.
You can also call 911 when you are not physically able to drive the person to the hospital, and the person has a condition that is growing worse.
When you call 911, an ambulance is sent with people trained in life support. The patient is taken to a hospital for emergency care. One reason to avoid using 911 if it’s not absolutely necessary is the cost. The patient or his or her insurance company will be billed for the ambulance, the hospital, and the doctor’s services. The best reason to use 911 only in a serious emergency is so that the emergency services personnel are free to help a person having a life-threatening emergency.
APS | CPS:
If you witness a life-threatening situation involving a senior or adult with disabilities, dial 911. Contact your local Adult | Child Protective Services agency any time you observe or suspect the following:
- Sudden inability to meet essential physical, psychological or social needs threatening health, safety or well-being
- Disappearing from contact with neighbors, friends or family
- Bruising or welts on the skin, especially those appearing on the face or lateral and anterior region of the arms (physically abused elders are much more likely to display bruises than seniors injured by accident)
- Fingerprints or handprints visible on the face, neck, arms or wrists
- Burns from scalding, cigarettes, or in shapes of objects such as an iron
- Cuts, lacerations or puncture wounds
- Sprains, fractures or dislocations
- Internal injuries or vomiting
- Appearing with torn, stained, bloody clothing
- Appearing disheveled, in soiled clothing or inappropriately attired for climate
- Appearing hungry, malnourished, disoriented or confused
Your Doctor:
If you think a person needs emergency treatment at a hospital, it’s sometimes helpful to first call your doctor for advice. Do this only if you have the time and the doctor is immediately available. If not, then you should call 911 or go to the nearest hospital. Your doctor can advise you as to whether an emergency situation actually exists.
If there is time to spare, then you should see your doctor first. Remember, a doctor’s visit won’t be as expensive as a hospital’s emergency treatment. And it won’t tie up vital emergency medical services. The doctor may also decide that the condition can be treated in his or her office or at home. This saves your time and the hospital’s time, and reduces overall health costs.
Hospital:
Doctors who specialize in emergency medicine see just about everything, from real emergencies to people who come in for minor problems because they have nowhere else to go. But hospital emergency treatment is expensive because of its 24-hour availability and high overhead costs.
So, when is it appropriate to go to a hospital? If you feel a person needs immediate attention and a primary care doctor isn’t available, then emergency care may be the best choice. Remember that emergency care is not first come, first served. Patients in the emergency room are treated according to the severity of their condition. This sorting of patients is called triage.
Other Options:
Urgent care centers. These doctor-staffed, walk-in medical facilities offer an alternative when there isn’t an emergency and you don’t have access to your personal doctor. They are generally more expensive than seeing your own physician but less expensive than an emergency room visit. The center usually has immediate access to simple laboratory procedures.
Poison control centers. People well trained to handle telephone calls dealing with poisoning emergencies staff these centers. Keep the number by your phone, especially if you have children at home.
Contact Supervisor
It is vital to maintain contact and seek counsel from your direct supervisor who in turn will seek advice and counsel from the TNS Admin Team. Each emergency must be immediately reported and documented properly. The safety of the individuals we serve is our utmost concern. This needs to be the single most important focus in any emergency that may arise.
____________________________________________
Introduction to Persons with Disabilities (ID, RC, ABI)
What Is an Intellectual Disability?
(ID)Intellectual disability is a disability that occurs before age 18. People with this disability experience significant limitations in two main areas: 1) intellectual functioning and 2) adaptive behavior. These limitations are expressed in the person’s conceptual, social and practical everyday living skills. A number of people with intellectual disability are mildly affected, making the disability difficult to recognize without visual cues. Intellectual disability is diagnosed through the use of standardized tests of intelligence and adaptive behavior. Individuals with intellectual disabilities who are provided appropriate personalized supports over a sustained period generally have improved life outcomes (AAIDD, 2011). In fact, many adults with intellectual disabilities can live independent, productive lives in the community with support from family, friends and agencies like The Arc.
How Many People Have Intellectual Disabilities?
An estimated 4.6 million Americans have an intellectual or developmental disability. Prevalence studies may not identify all people with intellectual disabilities. Many school age children receive a diagnosis of learning disability, developmental delay, behavior disorder, or autism instead of intellectual disability.
What Is Intelligence?
Intelligence refers to a general mental capability. It involves the ability to reason, plan, solve problems, think abstractly, comprehend complex ideas, learn quickly, and learn from experience. Intelligence is represented by Intelligent Quotient (IQ) scores obtained from standardized tests given by trained professionals. Intellectual disability is generally thought to be present if an individual has an IQ test score of approximately 70 or below.
What Is Adaptive Behavior?
Adaptive behavior is the collection of conceptual, social and practical skills that have been learned by people in order to function in their everyday lives. Significant limitations in adaptive behavior impact a person’s daily life and affect his or her ability to respond to a particular situation or to the environment. Standardized testing aims to measure the following skills:
- Conceptual skills: receptive and expressive language, reading and writing, money concepts, self-direction.
- Social skills: interpersonal, responsibility, self-esteem, follows rules, obeys laws, is not gullible, avoids victimization.
- Practical skills: personal activities of daily living such as eating, dressing, mobility and toileting; instrumental activities of daily living such as preparing meals taking medication, using the telephone, managing money, using transportation and doing housekeeping activities; occupational skills; maintaining a safe environment.
A significant deficit in one area impacts individual functioning enough to constitute a general deficit in adaptive behavior (AAIDD, 2011).
How Does Having a Disability Affect Someone’s Life?
The effects of intellectual disabilities vary considerably among people who have them, just as the range of abilities varies considerably among all people. Children may take longer to learn to speak, walk and take care of their personal needs, such as dressing or eating. It may take students with intellectual disabilities longer to learn in school. As adults, some will be able to lead independent lives in the community without paid supports, while others will need significant support throughout their lives. In fact, a small percentage of those with intellectual disabilities will have serious, lifelong limitations in functioning. However, with early intervention, appropriate education and supports as an adult, every person with an intellectual disability can lead a satisfying, meaningful life in the community.
How Can Supports Help?
Supports include the resources and individual strategies necessary to promote the development, education, interests, and well- being of a person. Supports enhance individual functioning. Supports can come from family, friends and community or from a service system. Job coaching is one example of a support often needed by a new employee with intellectual disabilities. Supports can be provided in many settings, and a “setting” or location by itself is not a support.
What Is the Definition of Developmental Disabilities (DD)?
According to the Developmental Disabilities Act (Pub. L. 106-402), the term developmental disability means a severe, chronic disability that:
- Is attributable to a mental or physical impairment or a combination of those impairments;
- Occurs before the individual reaches age 22;
- Is likely to continue indefinitely;
- Results in substantial functional limitations in three or more of the following areas of major life activity: (i) self care, (ii) receptive and expressive language, (iii) learning, (iv) mobility, (v) self-direction, (vi) capacity for independent living, and (vii) economic self-sufficiency; and
- Reflects the individual’s need for a combination and sequence of special, interdisciplinary, or generic services, individualized supports, or other forms of assistance that are of lifelong or extended duration and are individually planned and coordinated.
Before the age of ten, an infant or child with developmental delays may be considered to have an intellectual or developmental disability if his or her disabilities are likely to meet the above criteria without intervention.
How Does the DD Definition Compare with the AAIDD Definition of Intellectual Disability?
The major differences are in the age of onset, the severity of limitations, and the fact that the developmental disability definition does not refer to an IQ requirement. Many individuals with intellectual disability will also meet the definition of developmental disability. However, it is estimated that at least half of individuals with intellectual disability will not meet the functional limitation requirement in the DD definition. The DD definition requires substantial functional limitations in three or more areas of major life activity. The intellectual disability definition requires significant limitations in one area of adaptive behavior.
Those with developmental disabilities include individuals with cerebral palsy, epilepsy, developmental delay, autism and autism spectrum disorders, fetal alcohol spectrum disorder (or FASD) or any of hundreds of specific syndromes and neurological conditions that can result in impairment of general intellectual functioning or adaptive behavior similar to that of a person with intellectual disabilities.
Why Do Some People Still Use the Term “Mental Retardation”?
The term “mental retardation” is an outdated term that may offer special protections in some states, however, with the passage of Rosa’s Law in 2010, many states have replaced all terminology from mental retardation to intellectual disability. Although some still use the term “mental retardation” to be eligible for some services in a few states, in no case does having the label guarantee that supports will be available. The Arc does not encourage the use of nor promote the term mental retardation. The general public, including families, individuals, funders, administrators, and public policymakers at local, state and federal levels, are becoming aware of how offensive this term is and The Arc is actively working to make sure the public at large now use the preferred term of intellectual or developmental disability.
____________________________________________
Getting to Know the Client
TNS’s Getting To Know You client face sheet is an easy way to access key information regarding the clients we serve. These sheets contain the client’s allergies, diagnosis, emergency contacts and date of birth.
These sheets can be found within the staff binder assigned to work in direct care of the specific client.
____________________________________________
Person-Centered Thinking:
Understanding Why People Do the Things They Do
To support others in learning the skill of self-determination, individuals must be well able to listen to and understand human behavior. Comprehending the underlying functions of human behavior is critical to being able to adequately understand others. It must be understood that all human behavior is purposeful and goal-oriented, although the purposes or goals of each behavior may not be readily perceived. In fact, it is quite common to misperceive another’s purpose or goal. Understanding the many factors that influence human behavior and the way that behavior generally tends to present itself will guide one into greater understanding of others. The learner can begin to “listen” not only to words and body language, but also to the actual behaviors themselves, for the “message” behind those behaviors.
Discovering What Motivates People
When we discover what motivates people, we can support them in pursuing those activities.
Supporting people in what they want to do is what
self-determination is all about. When people can do what they like, they are
happier and have greater self-esteem. They can learn self-control. “To have meaning, find your passion and
pursue it.”
Some of these strategies are:
Help People Get a Life They Want. When people are actively engaged in a life that they like they are less likely to have behavior problems. When they are working toward goals that matter to them, they have less time and reason for behavior problems.
Identify Positive Behavior.
Identify the positive things the person is doing that help them to reach their own personal goals. This can include things like communicating, interacting with others, doing things without someone else suggesting them first, finishing tasks, and following instructions.
Identify Rewards.
Identify things the person finds rewarding. The purpose of this is not to find out what things to “take away” (punishment) from the person. Many people take this for granted, but it is often critical in the process of working with people we find challenging. Sincere praise is an underused reward. Praise can be communicated in many ways (one person counted over 100 ways) – from a bright smile, to a thumbs-up sign or a high-five.
Consistently reward positive behavior.
When working with people with challenging behavior, it is important to make sure the person is rewarded for positive behavior and that includes positive attempts.
We must reward effort and not just success or the effort will be very short lived. The frequency of rewards, recognition, and encouragement needs to be high.
The rule used in some of the most successful programs is 10 positive interactions (rewards, recognition, encouragement) for every 1 corrective/directive interaction.
Remember, however, that we must be working toward the day when the person can be rewarded more naturally for their positive behaviors.
Acquired Brain Injury (ABI) | Traumatic Brain Injury (TBI) RESOURCES
TBI
Traumatic brain injury occurs as the result of some external force being applied to the brain in an accident or trauma. As a result of this blow or rapid movement, the brain may be torn, stretched, penetrated, bruised or become swollen. Oxygen may not be able to get through to brain cells and there may be bleeding.
Diffuse axonal injury: The twisting motions or sudden changes in momentum that accompany some accidents may cause the bundles of nerve fibres to be stretched or shear. The term closed head injury is often used to describe this type of TBI, because the damage to the brain occurs as the result of these internal mechanisms, but usually with the skull remaining intact.
Penetrating injuries: This describes cases where some external object pierces the skull and comes in direct contact with the brain, thereby causing a TBI.
Other causes of brain trauma include falls, blows to the head, crushing injuries, electric shocks/ lightning strikes, and whiplash or violent shaking.
The common mechanisms of TBI include:
Acceleration/ Deceleration injuries: Refers to injuries in which the head is in motion and then abruptly comes to a halt. For example, if a car hits a tree, the car suddenly stops, and the driver’s head hits the steering wheel. The brain within the skull still has forward momentum and can hit the inner surface of the skull (which has bony edges) with some force, causing bruising, lacerations and bleeding.
Incidence
- Motor vehicle accidents (i.e. drivers, passengers, pedestrians, motor bikes, cyclists) are responsible for 70% of severe traumatic brain injuries.
- The peak incidence of TBI is among young males. 70% of TBI’s will involve young people aged between 16 – 24 years, and two thirds of those injured will be males.
- A second peak is observed after 75 years. But there are different causes for these two age groups. The main cause among young people is road crashes, whereas the main cause for the elderly is falls.
COMMON SIGNS AND SYMPTOMSCommon Signs and Symptoms
• Headaches
• Changes in sleep
• Dizziness
• Nausea/vomiting
• Fatigue
• Balancing Problems
• Sensory changes
• Slowed thinking
• Difficulty concentrating
• Memory problems
• Depression or anxiety
• Mood swings
Brain injury is unpredictable in its consequences. Brain injury affects who we are and the way we think, act, and feel. It can change everything about us in a matter of seconds.
The most important things to remember are:
- A person with a brain injury is a person first.
- No two brain injuries are exactly the same.
- The effects of a brain injury are complex and vary greatly from person to person.
- The effects of a brain injury depend on factors such as cause, location, and severity.
The human brain is magnificent and complex. The brain is made up of many parts, each with a specific and important function. It controls our ability to balance, walk, talk, and eat. It coordinates and regulates our breathing, blood circulation, and heart rate. It is responsible for our ability to speak, to process and remember information, make decisions, and feel emotions. Every brain is unique, ever-changing, and extremely sensitive to its environment.

The brain is divided into functional sections, called lobes:
- Frontal Lobe (shown in orange)
- Temporal Lobe (pink)
- Parietal Lobe (blue)
- Occipital Lobe (green)
- Cerebellum (red)
- Brain Stem (yellow)
Each lobe has an important and specific function, detailed below.
Frontal Lobes Functions (Orange)
Attention ConcentrationSelf-MonitoringOrganizationExpressive Language (Speaking)Motor Planning & InitiationAwareness of AbilitiesAwareness of LimitationsPersonalityMental FlexibilityInhibition of BehaviorEmotionsProblem SolvingPlanningJudgmentAn injury to the frontal lobes may affect an individual’s ability to control emotions, impulses, and behavior or may cause difficulty recalling events or speaking.Brain Stem Functions (Yellow)BreathingArousalConsciousnessHeart RateSleep & Wake CyclesThe brain stem controls the body’s involuntary functions that are essential for survival, such as breathing and heart rate.
Temporal Lobes Functions (Pink)
MemoryUnderstanding Language (Receptive Language)SequencingHearingOrganizationAn injury to the temporal lobes may lead individuals to demonstrate difficulty with communication or memory.Parietal Lobes Functions (Blue)Sense of TouchSpatial Perception (Depth Perception)Identification of Sizes, Shapes, ColorsVisual PerceptionIndividuals who have injured their parietal lobes may have trouble with their five primary senses.
Cerebellum Functions (Red)
Balance & CoordinationSkilled Motor ActivityVisual PerceptionAn injury to the cerebellum may affect balance, movement, and coordination.
Occipital Lobes Functions (Green)
VisionAn injury to one’s occipital lobes may lead to trouble seeing or perceiving the size and shape of objects.

The functional sections (lobes) of the brain are also categorized by side – the right side and the left side. If you split the brain down the middle into two equally-sized parts, they are not the same and do not carry the same functions. The right side of the brain controls the left side of the body, while the left side of the brain controls the right side of the body. Each side is responsible for different functions, and general patterns of dysfunction may occur depending on the side of the brain sustaining an injury.
The traits of each side are detailed below:
LEFT SIDE TRAITS
AnalyticalLogicalPreciseOrganizedDetachedLiteralInjuries of the left side of the brain can cause:Difficulties understanding language (receptive language)Difficulties in speaking or verbal output (expressive language)Catastrophic reactions (depression, anxiety)Difficulty speakingImpaired logicSequencing difficultiesDecreased control over right-sided body movements
RIGHT SIDE TRAITS
CreativeImaginativeIntuitiveConceptualEmpatheticFigurativeInjuries of the right side of the brain can cause:
Visual-spatial impairmentVisual memory deficitsLeft neglect (inattention to the left side of the body)Decreased awareness of deficitsAltered creativity and music perceptionLoss of “the big picture” type of thinkingDecreased control over left-sided body movements
An acquired brain injury (ABI) is an injury to the brain that is not hereditary, congenital, degenerative, or induced by birth trauma. Essentially, this type of brain injury is one that has occurred after birth. The injury results in a change to the brain’s neuronal activity, which affects the physical integrity, metabolic activity, or functional ability of nerve cells in the brain.
There are two types of acquired brain injury: traumatic and non-traumatic.
A traumatic brain injury (TBI) is defined as an alteration in brain function, or other evidence of brain pathology, caused by an external force. Traumatic impact injuries can be defined as closed (or non-penetrating) or open (penetrating).
Often referred to as an acquired brain injury, a non-traumatic brain injury causes damage to the brain by internal factors, such as a lack of oxygen, exposure to toxins, pressure from a tumor, etc. Read on for an overview of some of the common causes of brain injury.
| TRAUMATIC BRAIN INJURY CAUSES | NON-TRAUMATIC BRAIN INJURY CAUSES |
|---|---|
| FallsAssaultsMotor Vehicle AccidentsSports/Recreation InjuriesAbusive Head Trauma (Shaken Baby Syndrome)Gunshot WoundsWorkplace InjuriesChild AbuseDomestic ViolenceMilitary Actions (Blast Injury) | Stroke (Hemorrhage, Blood Clot)Infectious DiseaseMeningitisEncephalitisSeizureElectric ShockTumorsMetabolic DisordersNeurotoxic Poisoning (Carbon Monoxide, Lead Exposure)Lack of Oxygen (Drowning, Choking, Hypoxic/Anoxic Injury)Drug Overdose |
Brain injuries may be classified as traumatic or non-traumatic to describe the cause of the injury. They may also be classified as mild, moderate, or severe to indicate the initial severity of the injury. Other terms, such as diffuse or penetrating, may be used to describe the type injury. The most commonly used terms are shown below:
Diffuse Axonal Injury
A diffuse axonal injury can be caused by shaking or strong rotation of the head, as with shaken baby syndrome, or by rotational forces, such as with a car accident.
Concussion/Mild Traumatic Brain Injury (mTBI)
A concussion can be caused by direct blows to the head, gunshot wounds, violent shaking of the head, or force from a whiplash-type injury. Both closed and open head injuries can produce a concussion. A concussion is the most common type of traumatic brain injury.
Contusion
A contusion is a bruise (bleeding) on the brain caused by a force (blow or jolt) to the head.
Coup-Contrecoup Injury
Coup-contrecoup injury describes contusions that are both at the site of the impact and on the complete opposite side of the brain. This occurs when the force impacting the head is not only great enough to cause a contusion at the site of impact, but is also able to move the brain and cause it to slam into the opposite side of the skull.
Second Impact Syndrome
Second impact syndrome, also termed “recurrent traumatic brain injury,” can occur when a person sustains a second traumatic brain injury before the symptoms of the first traumatic brain injury have healed. The second injury may occur from days to weeks following the first. Loss of consciousness is not required. The second impact is more likely to cause brain swelling and widespread damage.
Penetrating Injury
Penetrating injury to the brain occurs from the impact of a bullet, knife, or other sharp object that forces hair, skin, bone, and fragments from the object into the brain.
Abusive Head Trauma (Shaken Baby Syndrome)
Abusive head trauma, also known as shaken baby syndrome, is a violent criminal act that causes traumatic brain injury. Abusive head trauma occurs when the perpetrator aggressively shakes a baby or young child. The forceful whiplash-like motion causes the brain to be injured.
Locked-in Syndrome
Locked-in syndrome is a rare neurological condition in which a person cannot physically move any part of their body aside from their eyes.
Open Head Injury
An open head injury, also known as a penetrating head injury, is a head injury in which the dura mater (the outer layer of the meninges) is breached. Penetrating injury can be caused by high-velocity projectiles or objects of lower velocity such as knives, or bone fragments from a skull fracture that are driven into the brain.
Closed Head Injury
A closed head injury is an injury to the brain caused by an outside force without any penetration of the skull. With a closed head injury, when the brain swells, it has no place to expand. This can cause an increase in intracranial pressure, which is the pressure within the skull.
(TNS does not own rights to the vidoes)
When working with people with ABI/TBI it is important to make sure that you know and understand the following:
Each individual with a TBI/ABI has gone through a traumatic experience that has drastically altered their day-to-day living. It is likely that they have been through hospitalizations, countless hours of tests and exams, physical therapy, and that their families have experienced devastation and heartache along the way. The following video helps us understand some of the process the individuals go through:
Immediately following a brain injury, two things occur:
- Brain tissue reacts to the trauma from the injury with a series of biochemical and other physiological responses. Substances that once were housed safely within these cells now flood the brain, further damaging and destroying brain cells in what is called secondary cell death.
- Depending on the severity of brain injury, effects may include temporary loss of consciousness or coma, respiratory (breathing) problems, and/or damaged motor functions.
Unlike what is seen in the movies, waking up following loss of consciousness is not immediate and sometimes can be quite difficult for the individual and their loved ones. It is important to be aware of the various neurologically-based symptoms that may occur during this period, such as irritability, aggression, posturing, and other issues. Post-traumatic amnesia (PTA) is also typically experienced as an injured person regains consciousness. PTA refers to the period when the individual feels a sense of confusion and disorientation (i.e., wondering who or where they are and what has happened to them) and an inability to remember recent events.
As time passes, these responses typically subside, and the brain and other body systems approach stability. Unlike bones or muscle tissue, the neurons in the brain do not mend themselves. New nerves do not grow in ways that lead to full recovery. In fact, certain areas of the brain remain damaged, and the functions that were controlled by those areas may be disrupted and lead to challenges in the individual’s life.
It is important for individuals to continue living life with optimism, positivity and in a progressive direction. It may take some time for the families and individuals to adapt, but overall, with support, the individuals and families are able to connect and interact in ways that help them improve their quality of living and find renewed passion for life. Families ache for their loved ones to be able to resume “normal” life functionality, and this will likely take adaptations and adjustments to help them progress. It is our job to focus on the individuals goals and PCSP plan to help them progress in the ways that both the individual and family see fit.
It is likely that as a staff you will enter someone’s life during a time that they are striving to continue to develop and find adaptations to get back into activities and things they once enjoyed doing before. Always be aware of the individual’s overall journey and take the time to be patient in helping them with patience and understanding. Your greatest area of help will be with positive outlook and helping the individual continue to look to the future in positive ways. The video below shows one individual’s story of regaining a purpose filled life, believing progression is an option even against all odds.
As you work with ABI/TBI individuals, compassion and persistent support help individuals overcome their most difficult challenges in life. It is extremely important for continual observation and adaptation as a necessary step in the success of the supports we provide. Balance, communication, eating, and other processing skills may be a minute by minute need to ensure safe and appropriate support. It is never appropriate to neglect an individual’s support needs. This is our top priority at True North Supports, to provide proficient supports that include awareness and adaptations to help the individual maintain health and safety at all times during our shifts..
The severity of damage to the brain after an injury is the primary factor in predicting the injury’s impact on the individual. Brain injury is typically categorized as mild, moderate, or severe.
| MILD BRAIN INJURY | MODERATE BRAIN INJURY | SEVERE BRAIN INJURY |
|---|---|---|
| Brief, if any, loss of consciousnessVomiting and DizzinessLethargyMemory Loss | Unconsciousness up to 24 hoursSigns of brain traumaContusions or bleedingSigns of injury on neuroimaging | Unconsciousness exceeding 24 hours (coma)No sleep/wake cycle during loss of consciousness (LOC)Signs of injury appear on neuroimaging tests |
A severe brain injury may cause the individual to experience an unconscious state, where one appears to be in a deep sleep and cannot be aroused or respond purposefully. Assessments will typically reveal that the individual has no sleep and wake cycles. This loss of consciousness (LOC) is referred to as a coma. Depending on varying factors and the severity of injury, the individual may remain in a coma, emerge from a coma, or experience an increased level of consciousness.
A person who is truly in a coma will not be considered for any type of brain injury rehabilitation program. People can, however, experience different states of consciousness after brain injury. Understanding these disorders of consciousness can be important when discussing treatment and possible rehabilitation options.
Vegetative State
An individual is unaware, but begins to have sleep and wake cycles; normal digestion, breathing, and heart rates; and may open his or her eyes. The individual may occasionally respond to stimuli.
Persistent Vegetative State
Doctors consider a person to be in a persistent vegetative state one year after traumatic brain injury or three to six months after a hypoxic or anoxic brain injury.
Minimally Conscious State
An individual shows slight but definite self-awareness or awareness of their environment.
Locked-in Syndrome
An individual can only move his or her eyes, not any other part of their body, and is conscious and able to think.
Brain Death
A person with brain death is not alive because all the brain functions, including the brain stem, no longer work.
In Summary
Just as no two people are exactly alike, no two brain injuries are exactly alike. For some, brain injury is the start of a lifelong disease process. Brain injury requires access to a full continuum of treatment and community-based supports provided by appropriately educated clinicians serving on an interdisciplinary treatment team.
The individual who sustains a brain injury and his or her family are the most important members of the treatment team. Their choices, goals, and backgrounds must always be taken into consideration in treatment planning.
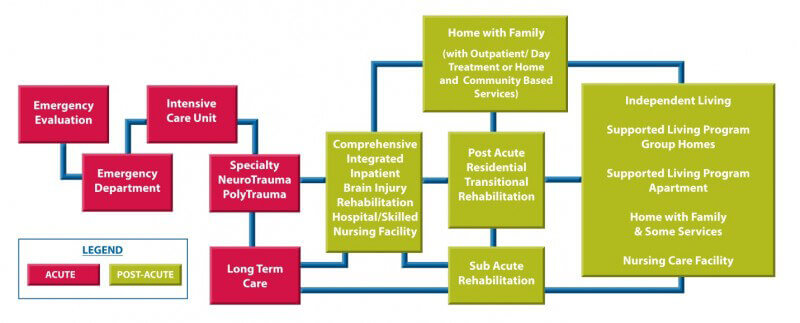
The diagram above depicts brain injury treatment in an orderly progression from trauma care to community integration. Individuals who sustain brain injuries may enter, exit, and re-enter treatment at any point along the continuum. Treatment may be needed continuously or on an intermittent basis throughout the individual’s life.
We provide vital support to individuals who have had a traumatic brain injury. Knowing and understanding the individual, their continuum of care (support plan) and how to best help the individual and their family will allow our supports to be very effective and very helpful in the overall quality of life for the individual and their loved ones. Knowing that they have a staff like you and a company like TNS on their team will provided longterm dividends that are invaluable for everyone involved.
**Information and materials gathered from The Brain Injury Association of America.**
____________________________________________
Quality Management Plan
TNS has implemented a strategic grievance plan in order to resolve the majority of problems and concerns in a safe and effective manner. All grievances and complaints will be kept confidential to protect the interest of all parties.
Residents, advocates/and or host parents who have reason to believe that a resident/client or staff has been unfairly treated while taking care of the needs of a client. They are also responsible to report any unauthorized persons allowed in the home. The following plan has been put in place to ensure that a proper resolution will satisfy all parties involved as well as prevent future incidents from occurring within the company.
If an incident occurs within the home or community that warrants an incident | behavior report such as, police being contacted, theft, bodily harm, lost client, seizure, soar restraint, med error, emergency room visit, sexual harassment and/or any incidents where someone is uncomfortable, or the loss of client’s confidential information. An incident report will be filled out and TNS will do an investigation to get all of the facts to resolve the matter as quickly and thoroughly as possible. If any of the following occur, staff is to contact their direct supervisor immediately along with filling out an incident | behavior report.
This incident report will be sent to TNS Admin who will review the case.
Process and Record Complaints
- Log the complaint on an incident report
- Notify Direct Supervisor
- TNS Admin Team will review case and gather facts
- Suspension will be given to staff if deemed appropriate by Director.
- Suspension and or movement of staff or client for objectivity and Safety during the formal review process
- Talk to the involved parties, by phone or in person
Investigate and Analyze the Complaint
- Get all facts from all parties involved
- Keep records in the complaint file of all meetings, conversations or findings
- Forward the complaint to the appropriate level of authority for resolution
- Notify the client and staff promptly of a proposed resolution
- Develop an action plan for incident prevention and have necessary parties sign
Follow-Up
- Follow up two weeks after incident with affected parties and ensure that action plan and goals are carried out
- If the incident was not resolved internally it will go before the human rights committee for immediate review
The commitment and continuing involvement of company management is critical to successful complaint resolution and to the optimum use of complaints as a management tool. Supervisors will help discover new ways to improve both the complaint-management system and the fairness of remedies offered to clients and staff alike.
The following will be used after all incidents are either resolved or turned over to the Human Rights Committee.
| YES | NO | Comments | |
| Was an incident report filed? | |||
| Did all parties involved resolve the incident? | |||
| Was local law enforcement involved? | |||
| Was anyone hospitalized? | |||
| Were any moneys involved and was it restored to the proper party? | |||
| Was the staff relocated or terminated? | |||
| Did the incident go to the human rights committee? | |||
| Was an action plan or contract put in place to prevent similar incidents from happening again? |
Plan of Correction
If TNS is found to be out of compliance for any reason it will immediately address and resolve any and all issues that arise. TNS will respond to the necessary authorities within the specified time frame that DSPD gives them. All compliance issues will be directed to our TNS Admin Team – who will oversee any and all methods of correction and will responsible for assigning tasks to qualified team members to ensure that all corrections are made in a timely manner and with the highest standards.
Emergency Management & Business Continuity
** Individuals in Supported Living and Supported Employment Settings**
All individuals in Supported Living and Supported Employment settings will have a Individual Emergency Preparedness Plan developed to meet their specific needs.
This plan is reviewed annually. Each individual in Supported Living and Supported Employment needs to assume the primary responsibility for his/her care during an emergency. Provider staff will work with the individual and/or their family in development and execution of the Plan. In the event of an emergency, provider staff will attempt to contact individuals in Supported Living settings as quickly as it possible to assess their needs. Supported Employment staff will work with the individual’s employer in the development of a basic emergency plan to be implemented should an emergency occur during the working day.
Content for Individual Emergency Preparedness Plan: (These are items that will possibly be included in the individual’s Personal Emergency Plan. It is staff responsibility to execute each item found on the individual’s emergency preparedness plan.)
- Establish a Personal Support Network: (A personal support network is made up of individuals who will check with the individual in an emergency to ensure that the individual is okay and give assistance if needed. This includes identifying a minimum of three people per location where the individual spends a signification part of their week: job, home, volunteer site etc.)
- Help the individual organize a network for their home, workplace, and other place where they spend a lot of time.
- Give the network members copies of the individual’s emergency information list.
- Arrange with the network to check on the individual immediately after an emergency strikes.
- Agree and practice a communications system regarding how to contact each other in an emergency.
- Show the network members how to operate and safely move the equipment the individual uses for their disability.
- Explain to the network any assistance for personal care the individual may need.
- The individual and their network members should always notify each other when they are going out of town and when they will return.
- Help the individual develop a Health Card, which contains emergency health information.
- Help the individual to maintain at least a 7 to 14 day supply of essential medications. (If not possible, at least a three day supply)
- Help the individual develop an emergency contact list including a number of someone who lives outside of the area.
- Help the individual gather necessary emergency documents. (Records, social security card, identification cards, bank accounts, etc.)
- Help the individual conduct an “Ability Self-Assessment” to evaluate their capabilities, limitations, and needs, as well as their surroundings to determine what type of help will be needed in an emergency.
- Help the individual develop a 72-hour emergency kit and obtain necessary supplies to use in the event of an emergency.
Emergencies will happen. It is important that each individual we support has a proper plan in place to address specific emergencies that may arise.
TNS staff on shift are responsible for the individuals in their supervision during crisis and emergency situations. It is likely most individual plans will require reunification of the individual with their families. Before transitions are made, TNS’ number one concern is the safety and welfare of the staff and the individual. Make emergency contacts as presented in the individual’s personal EM plan and contact supervisors for direction as needed.
Do not fear or panic, stay calm and communicate openly. TNS admin and supervisors will help and advise throughout the entirety of the incident. TNS admin will help as needed.